Flint Office
1303 S. Linden Rd., Suite D
Flint, MI 48532

Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.

Hammertoe is a foot deformity that affects the toes, causing them to bend or curl unnaturally at the middle joint, resembling a hammer's shape. This condition can cause discomfort, pain, and difficulty in finding comfortable footwear. Causes of hammertoe include wearing ill fitting shoes, especially high heels or shoes with a narrow toe box. These types of shoes can force the toes into an abnormal position over time. Genetic factors, arthritis, or nerve damage can also contribute to the onset of a hammertoe. Early intervention can often prevent the condition from worsening. Non surgical treatments include wearing shoes with a wide toe box, custom orthotics, or splints to help straighten the toes. In more severe cases, surgical intervention may be necessary to straighten the affected toe. If you have developed a hammertoe that is causing pain, it is suggested that you make an appointment with a podiatrist for an evaluation and appropriate treatment options.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists from Community Podiatry Group. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact our office located in Flint, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
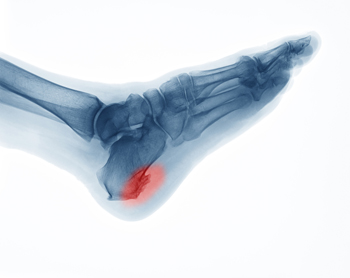
Heel spurs, or osteophytes, are extra bone growths on the heel bone that can cause pain and discomfort. Although only 5% of people with heel spurs experience pain, they can develop from conditions like plantar fasciitis or arthritis, leading to inflammation and pressure on the heel. Exercises can help increase flexibility in the plantar fascia and strengthen foot muscles to reduce inflammation and alleviate pain, though they will not make heel spurs go away. Such exercises include the big toe stretch, calf stretches, golf ball rolls, and more. The big toe stretch involves crossing the affected leg over the opposite leg, gently grabbing the big toe between the thumb and index finger, and slowly pulling the big toe upward until a stretch is felt on the bottom of the foot. Calf stretches are done by standing facing a wall with the hands placed on the wall at shoulder height and stepping the injured foot back about 18 inches. The heel should be flat on the ground and the front knee bent forward. Slowly lean forward until a stretch is felt along the back calf. For the golf ball roll, sit in a chair with a golf ball placed under the bare foot and roll it from the ball of the foot to the heel several times. Other treatments for heel spurs include wearing orthotics, night splints, steroid injections, or in severe cases, surgery. If you have a painful heel spur, it is suggested that you make an appointment with a podiatrist for treatment tailored to your needs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Community Podiatry Group. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Flint, MI . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.

The strong band of tissue that runs from the calf muscles to the heel bone is known as the Achilles tendon. When this tendon is overused, which is frequent among runners, dancers, and other athletes, it can become inflamed and extremely painful. This condition is called Achilles tendinopathy. The top cause of Achilles tendinopathy is overuse, which tears or stretches the tendon and causes inflammation. Other causes include certain types of arthritis, flat feet, and overpronation. In addition, wearing shoes that lack adequate support, being overweight, and taking certain antibiotics may increase the likelihood of developing Achilles tendinopathy. There are a number of treatments available for Achilles tendinopathy, but healing time depends on the severity of the injury. In some cases, surgery is required. There are several ways to prevent tendinopathy, including stretching exercises and warmup and cool-down routines. Wearing proper footwear is another way to help prevent this injury. For more information, it is suggested that you consult a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Community Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Flint, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.

The feet are responsible for providing balance, mobility, and a steady base for the body. They also serve as shock absorbers while walking and running, and provide cushioning for the body. Each foot has 26 bones, several tendons, ligaments, and muscles that are naturally coordinated to function together. The muscles and tendons are categorized into two groups, labeled intrinsic and extrinsic. The muscles that start in the lower leg and wrap around the ankles before they attach to the foot are called the extrinsic muscles. The other group of muscles that are known as the intrinsic muscles begin and end in the foot. These muscles are layered along the bottom of the foot to form the arch. These groups of muscles work in harmony while walking and running and are not given much thought as it happens naturally. There are abnormal foot structures that can alter the natural alignment of the bones. People who have flat feet, babies that are born with clubfoot, or people who stand for long periods may develop chronic foot conditions. If you would like more information about how the feet are constructed, it is suggested that you speak with a podiatrist.
If you have any concerns about your feet, contact one of our podiatrists from Community Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Flint, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics and its related study deal with the forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
Biomechanics and its related study deal with forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
The history of studying biomechanics dates back to ancient Egypt at around 3000 B.C., where evidence of professional foot care has been recorded. Throughout the centuries, advances in technology, science, and an understanding of the human body led to more accurate diagnosis of conditions such as corns for example. In 1974, biomechanics garnered a large audience when Merton Root founded Root Lab to make custom orthotics. He proposed that corrections of certain conditions could be implemented to gain strength and coordination in the area. Due to his research, we still use his basic principle of foot orthotics to this day.
As technology has improved, so have the therapeutic processes that allow us to correct deficiencies in our natural biomechanics. Computers can now provide accurate readings of the forces, movements, and patterns of the foot and lower leg. Critical treatment options can be provided to patients now who suffer from problems that cause their biomechanics to not function naturally. The best results are now possible thanks to 3D modeling and computing technologies that can take readings and also map out what treatment will do to the affected areas.
These advanced corrective methods were able to come to light thanks to an increase in both the technologies surrounding biomechanics and also the knowledge of how they work naturally. For example, shoe orthotics are able to treat walking inabilities by realigning the posture deviations in patients caused by hip or back problems. Understanding foot biomechanics can help improve movement and eliminate pain, stopping further stress to the foot. Speak with your podiatrist if you have any of these problems.